COVID-19 and primary health infrastructure: Is rural India in ruins?
June 15, 2020 | Monday | Views
The coming weeks and months are challenging for India
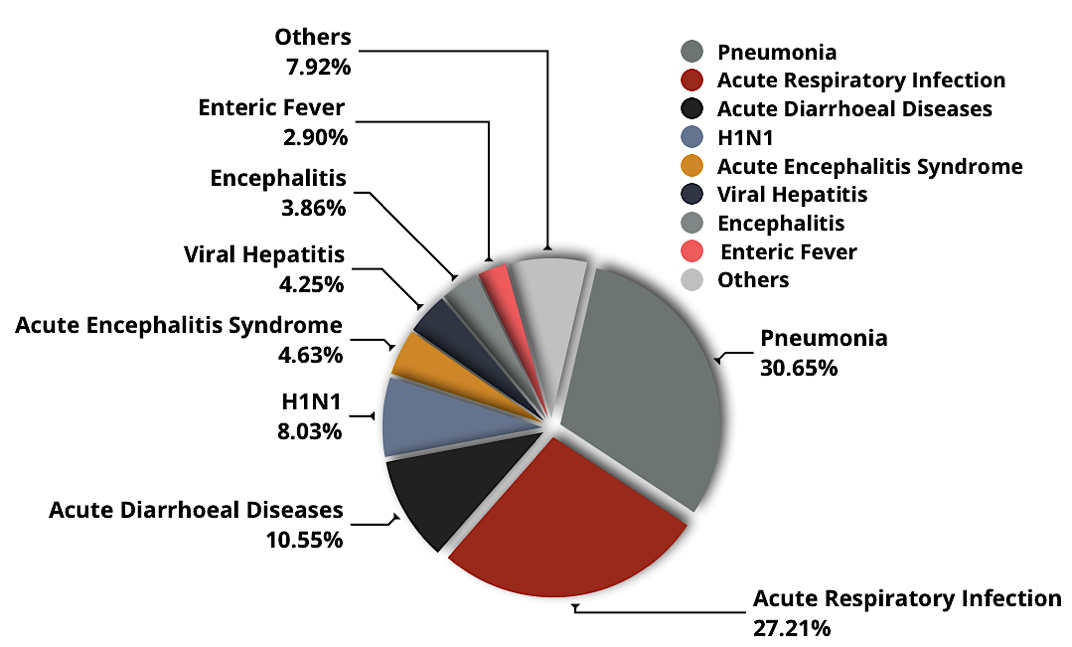
(Proportion of deaths due to infectious diseases- National Health Profile, 2019, Central Bureau of Health Intelligence)
The novel coronavirus 2019 has taken the world by a storm and brought life to a standstill. Caused by the SARS-CoV-2 virus, the disease presents as mildly symptomatic in most afflicted individuals, with possibilities of complications in those with co-morbidities. The devastation does not end there. The socio-economic landscape of the world has suffered irrevocable damages, particularly, in developing nations such as ours. A dearth of essential resources and an ineffective workforce, make it unlikely for India to be rescued from the impending doom in time.
Rural India, as stated by Dr. Soumya Swaminathan, WHO’s Chief Scientist, may become the next coronavirus epicentre. Lack of social distancing, temporary unemployment, poor health infrastructure, restricted activities of rural health workers, misinformation and confusion, deficient water and sanitation facilities altogether may turn rural regions into COVID-19 hotspots. This opportunity should be utilised to strengthen the country’s primary health care system. Although an impossible feat under current time constraints, the right steps in this direction will definitely help in the future.
We need to understand the overall health scenario of our country. Deaths in India due to Communicable Diseases are higher than the Global Average (IHME, Global Burden of Disease 2017). Expenditure on Healthcare by different sectors is alarmingly low. Maximum share of health expenditure in India, including rural areas is ‘Out of Pocket’ expenses, one of the highest compared to other countries. Contagious Respiratory Diseases in India account for more than 50% of total deaths. Rural regions that support 70 % of the Indian population, lacks enough health facilities or manpower in many aspirational districts demarcated by the Government.
In a country whose foundations rely upon a major fraction of workers earning wages on a daily basis without insurance and adequate savings, the economic scenario is unstable. Migrants exasperated with their emotional turmoil have taken to the roads. This may exacerbate the situation by increasing chances of widespread transmission. Information about their exposure and status of infection is extremely limited. Guidelines have been stated in many tertiary medical colleges, regarding the screening and quarantine of incoming labourers.
However, these rely on them approaching the hospital authorities and revealing their travel history. This is very unlikely to happen considering their mindset and the stigma surrounding the disease. As a result, thousands of cases will go unnoticed, and community transmission through the asymptomatic carriers among the migrants may increase rampantly. With the lack of proper scientific temper in our country, these serve as added burdens to an already frail health system.
Healthcare facilities are underfunded to support current demands, hampering most provisions. The primary health care centres and lower tiers in rural regions are involved in spreading awareness regarding infectious diseases such as dengue, malaria, tuberculosis among others, through home visits by health workers. Maternal and child-care duties, such as antenatal and postnatal care are also disseminated through the same medium.
“Recently, due to the outbreak, all such activities have come to a complete halt. Despite orders to normalize the situation from authorities, most rural areas are still deprived of these programs, highlighting one of the many failures of our health system.”, says Dr. Somajita Chakraborty, HOD, Obstetrics and Gynaecology, Diamond Harbour Medical College and Hospital, West Bengal. Rural morbidity and mortality are mainly associated with respiratory and water borne diseases that are preventable. However, the COVID-19 emergency has diminished all regular actions of identification and prevention.
Until recently, India had only 126 government based COVID-19 testing centres to handle a population of over 1.35 billion people (ICMR, April 2020). The surveillance in our country is hindered by a severe lack of awareness. Reports of patients trying to flee from isolation wards and conceal their travel records have been rampant. Lack of proper intervention on the part of hospitals have been noticeable. In fact, there is sceptic evidence on incorrect results being released and numbers being withheld. Rural population is at the verge of poverty, uncertainty and ill health. Without rigorous monitoring of asymptotic COVID cases by grass root workers and a strong referral system, it would be impossible to check spread of the virus. Incidence of catastrophic expenditure due to health care costs will offset the gains of income, further questioning the Government schemes aiming to reduce poverty.
Most hospital facilities in districts lack state-of-the-art infrastructure to address emergencies such as this. Although by now, much of the mayhem and tumult has considerably subsided, we do need to remember that the Indian health system deserves immediate attention. A severe shortage of adequately trained staff has rendered us helpless to contain the infection, particularly in densely populated states and low-resource regions, which India is replete in. We are highly deficient in health care services as per the recommended levels advisable by the World Health Organization.
Challenges are discernible at every turn and the dream of a fruitful health order today, seems no less than a mirage. The coming weeks and months are challenging for India and we need to take strong measures to meet this emergency and its inevitable aftermath.
Sukanya Chakraborty1 , Aparajita Chattopadhyay2
- Indian Institute of Science Education and Research, Berhampur
- International Institute of Population Sciences, Mumbai