What’s dampening the Global AMR Battle?
December 01, 2024 | Sunday | Features | By Mansi Jamsudkar
Although significant national and worldwide efforts have been undertaken to provide financial incentives for antibiotic research and development, it is still unclear how best to fortify the existing programmes to spur antibiotic innovation further. The incentive programmes in place now are a crucial first step in enhancing the economic viability of antibiotic development. However, it seems like there isn't enough global coordination among all the programmes, which could lead to duplication of effort, funding gaps in the value chain, and the failure to include crucial AMR objectives. Let’s dig deeper.
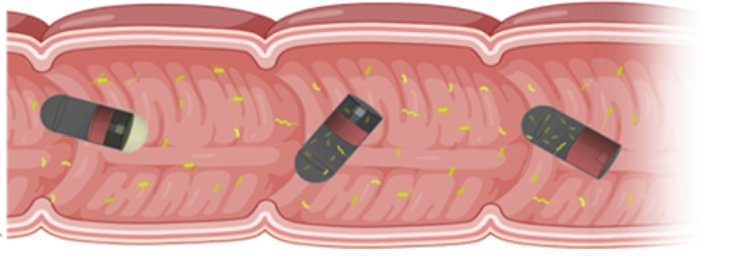
image credit- shutterstock
Antimicrobial resistance (AMR) is a growing global concern, with the situation worsening year by year. The speed of developing resistance is at par or, in fact, more than the speed of novel antibiotic development. Most of the big pharmaceutical companies have left antibiotic research due to the high risk of failure and poor return on investment. Antibiotic research is mostly carried out by academic institutes and small- and medium-sized enterprises. However, they lack sufficient funds to take the compounds from early and mid-stage to clinical trials and market.
Insufficient funding remains a major challenge in advancing research on AMR, both in India and globally. The funding landscape for AMR research is characterised by a lack of sustained investment and inadequate financial support from both the public and private sectors. This lack of resources significantly hampers the development of new antibiotics, diagnostic tools, and treatment approaches. In a scenario where countries fail to contain drug resistance, we could face a staggering $1.7 trillion annual reduction in global economic output by 2050, amounting to a 0.88 per cent decrease in GDP. This would not only escalate hospital treatment costs but also adversely affect tourism and domestic hospitality.
An annual investment of $63 billion spent improving access to, and developing new antimicrobials, could generate more than $1.7 trillion in benefits a year by 2050. While $63 billion may sound like a lot of money—in reality, it’s less than the world spends on cosmetic surgery, less than video gamers spend on in-game purchases, each year—and it’s about an eighth of what the world spends on takeout coffee. These findings are from the recent report from Center for Global Development, based at Washington DC and London, a think tank that uses economic research to reduce global poverty and inequality.
“Scenario that promotes increased access to high-quality treatment for bacterial infections, coupled with funding that spurs the development of new gram-negative antibiotics, presents a more hopeful future. Such initiatives could boost the global economy by an estimated $960 billion by 2050, while simultaneously reducing health care costs by $100 billion. This is in addition to the benefits of simply improving people’s lives and the insurance value of reducing the risk of an AMR outbreak. Inaction on AMR carries a significant economic burden. However, the potential economic gains from measures that stem the rise of AMR are substantial,” said Mark Plant, Chief Operating Officer and Senior Policy Fellow, the Center for Global Development, USA.
In India, funding for AMR research and initiatives has been relatively limited compared to the need. Public and private sector investments in AMR research have been insufficient, with most resources directed towards modifying existing antimicrobial compounds rather than discovering new therapeutic agents.
Misalignment of incentives
Only a handful of countries have addressed the AMR issue by implementing or proposing financial incentive models to promote antibiotic innovation. In India, many initiatives towards financial incentives have been made which include the UK-India Fleming Fund (a partnership between the Fleming Fund and India's Ministry of Health and Family Welfare. The fund's goal is to accelerate collaboration on AMR surveillance across One Health sectors), a partnership between C-CAMP and CARB-X that provides funding opportunities for Indian medical innovators working on AMR, Grand Challenges India, etc. However, the misalignment of these incentives is not allowing the achievement of desirable AMR goals in India.
“One important hurdle is misalignment of incentives. While governments and health services are incentivised to promote prudent use of this common good, pharmaceutical companies are incentivised to increase the volume of sales to maximise profits. This problem must be addressed or else the major efforts going into developing new antibiotics will be in vain,” opined Olof Lindahl, Project Coordinator at Uppsala Antibiotic Center, Uppsala University, Sweden.
The disconnect between costly antibiotic development and low net present value (NPV, a value calculated based on ultimate costs and revenue) stresses the need for financial incentives that can either decrease the cost of R&D or increase the market revenues. Therefore, several global organisations have put forward funding strategies to lower the cost of developing an antibiotic, directly or indirectly, by cutting down the risk of failures, as they cover both successful and unsuccessful projects. Of the major financial incentives in the field of antibiotic R&D, 71 per cent are strictly push incentives funding the development of novel antibiotics. For instance, the flourishing preclinical antibiotic pipeline in Europe (52 per cent) and America (35 per cent) can be attributed to the proactive approach of government and non-government philanthropic organisations in these continents.
Although these strategies showed a positive impact on NPV, they are insufficient as they do not cover the revenue generation after antibiotic approval and are inadequate alone to recuperate the dried antibiotic arena. Dr Reeta KH, Professor at All India Institute of Medical Sciences (AIIMS), Delhi said, “Equal attention to market sustainability through pull incentives is needed after antibiotic approval to mitigate the market failure challenges, as evidenced by the bankruptcy of Achaogen, an SME that developed plazomicin. Achaogen was unable to sustain the market of plazomicin despite being push-funded from initial stages to clinical trials by Wellcome Trust, the National Institute of Health (NIH), and the Biomedical Advanced Research and Development Authority (BARDA).”
Revitalising the antibiotic pipeline through financial assistance in the form of push funding and uniting the scientific community can bring back the lost art of discovery. Various push funding mechanisms in the last decade have tried to narrow the discovery void that occurred after the lucrative 1980s era of antibiotic development. However, despite numerous funding mechanisms, the pace of development is still slow, and the antibiotic market is unattractive for the big pharmaceuticals. Along with push funding, there is a need to incentivise antibiotic developers through pull funding after regulatory approval to sustain the market.
Pharma’s apathy towards AMR R&D
Indian pharmaceutical companies have significantly reduced investments in AMR research due to several interconnected factors. Developing new antibiotics is less profitable compared to other therapeutic areas like chronic diseases or lifestyle drugs. Antibiotics are usually prescribed for short durations, making their market potential smaller than drugs for chronic conditions, which have long-term usage and higher sales volumes. Moreover, the Indian pharmaceutical industry is highly competitive, with a focus on producing generic drugs at lower costs. Investing in new antibiotic research is seen as less lucrative because generic drugs dominate the antibiotic market, making it difficult for new, more expensive antibiotics to gain traction.
Even if a new antibiotic is successfully developed, it is often reserved for severe cases to prevent the development of resistance, leading to limited usage. This controlled application reduces sales potential, discouraging companies from investing in AMR research. Furthermore, Global efforts to limit the overuse of antibiotics further decrease the potential returns on investment for pharmaceutical companies. Policies that encourage the prudent use of antibiotics make it difficult to recoup the significant costs associated with research and development.
While commenting on the need for action from pharmaceutical companies, Marijn Verhoef, Director of Operations and Research, Access to Medicine Foundation, Netherlands said, “Tackling the sheer scale and pace of drug resistance is a complex global health issue that will require action from pharmaceutical companies across several areas. This includes providing appropriate access and implementing stewardship measures to safeguard the effectiveness of innovative antimicrobials. Failure to do this will limit efforts to tackle drug resistance.”
The hesitance in investments by Indian pharmaceutical companies in AMR research is largely driven by economic considerations, scientific challenges, lack of robust incentive structures, and a focus on more profitable therapeutic areas with few approval processes and no need for extensive clinical trials. To reverse this trend, there needs to be stronger government support, global collaboration, and innovative funding models that can make AMR research a financially viable venture for these companies.
Why the urgency?
According to the United Nations Environment Programme (UNEP), up to 10 million deaths per year could occur by 2050 due to AMR. "The threat of AMR is not just theoretical; it's something we're seeing every day in our ICUs. Patients who would have had a fighting chance just a few years ago are now facing infections we struggle to treat. We need new weapons in our arsenal, and we need them now. While the development of new antibiotics is crucial, we cannot neglect the importance of antibiotic stewardship. By using these life-saving drugs responsibly and implementing effective infection control measures, we can help slow the spread of resistance." shared Prof. Dr Rahul Pandit, Chair Critical Care, Sir HN Reliance Foundation Hospital, Mumbai.
Although major international and national initiatives are aimed at financially incentivising the research and development of antibiotics, it remains unclear how to effectively strengthen the current set of incentive programmes to further accelerate antibiotic innovation. The current set of incentive programmes is an important initial step to improving the economic feasibility of antibiotic development. However, there appears to be a lack of global coordination across all initiatives, which risks duplicating efforts, leaving funding gaps in the value chain and overlooking important AMR goals.
In conclusion, we can say that there are significant holes in the global incentive scheme that will impede progress towards bringing novel antibiotics to the market. Firstly, the majority of R&D funding focuses on early-stage push incentives aimed at basic research and preclinical trials, while late-stage push incentives for clinical development remain limited. Secondly, there is a significant lack of large-scale pull incentives that effectively stimulate private investment in clinical trials and the commercialisation of antibiotic products. Thirdly, key public health policies, which outline target product profiles, sustainability goals, and patient access considerations, are not well-integrated into existing R&D incentive frameworks.
Lastly, there is a lack of comprehensive guidance and coordination among the various initiatives currently in place. This fragmented approach could be a major factor contributing to gaps in the incentive structure and unmet public health needs. Establishing an international coordination and governing body to support national implementation could be a crucial step toward addressing these policy issues. At the national level, countries must reassess their funding strategies to better drive antibiotic innovation in response to the urgent global threat of AMR. High-level commitments need to be transformed into concrete actions across all sectors.
Recent developments in Indian AMR space
- Innominds, a US-based digital transformation and product engineering company, partnered with Hyderabad-based startup SCIINV Biosciences to introduce AMRx, an advanced AI/ML-driven digital diagnostic tool designed to combat the growing threat of AMR (June 2024).
- The Indian Medical Association (IMA) formed the National Alliance of Medical Professionals on Antimicrobial Resistance (NAMP-AMR) (July 2024).
- Hyderabad-based Bharat Biotech collaborated with US-based Alopexx, Inc., for the co-development and commercialisation of Alopexx’s proprietary broad-spectrum anti-microbial vaccine, AV0328, in India and other low-income and lower-middle-income countries (September 2024).
- Orchid Pharma, a Chennai-based company, formed Orchid AMS (Antimicrobial Solutions), a dedicated division focused on helping address the critical challenge of AMR in India (September 2024).
- Telangana launched the AMR Action Plan (October 2024).
- The International Centre for Antimicrobial Resistance Solutions (ICARS) signed a partnership with the Centre for Cellular and Molecular Platforms (C-CAMP), under the aegis of the India AMR Innovation Hub (IAIH), to tackle the growing threat of AMR across the One Health domain (October 2024)
Can the academic sector provide robust solutions to counter AMR by driving innovative research?
Dr Aakanksha Kalra, Assistant Professor, Shoolini University
Resistance to existing drugs has been observed even before the discovery of antibiotics, particularly against natural agents such as plant extracts. After the discovery of penicillin in 1928, the first instances of antibiotic resistance were documented during World War II in the 1940s. However, it wasn’t until 2016 that antimicrobial resistance (AMR) garnered significant political attention, leading to the establishment of National Action Plans and stewardship programmes in over 170 countries. Despite this, by the end of 2024, less than 20 per cent of these programmes have been adequately funded or implemented. Meanwhile, the emergence and rapid spread of AMR has continued, driven by factors such as the misuse and improper disposal of antibiotics, environmental conditions, and the role of various agents like soil, water, and animals in spreading resistant genes. This has created a significant gap between the rising threat of AMR and the mechanisms in place either to prevent or to combat it.
Addressing AMR effectively requires a multifaceted approach focusing on three key areas: assessment of AMR’s current status and spread, accurate diagnosis of resistance mechanisms, and development of both improved treatments and novel technologies. Although AMR remained underappreciated for many years, the post-COVID era has brought renewed attention to the issue. The foremost priority understands the current spread of AMR, which is being actively studied by researchers worldwide. This includes tracking the spread of pathogenic infections, identifying resistance genes, and understanding resistance mechanisms across different regions at regular intervals.
Recent academic research has highlighted new pathways for AMR transmission, such as ocular infections, the gut microbiome, disinfectants and antiseptics, and plastics, which represent critical areas of concern. Additionally, understanding microbiome dynamics as predictors of disease resolution during antibiotic treatment of chronic infections has emerged as a promising avenue in combating resistance. Novel contributors to resistance, such as extracellular vesicles (EVs), along with established agents like plasmids and integrons, have also been identified. While improving existing antibiotic therapies remains essential, the development of innovative technologies is crucial to address the growing challenge of AMR.
Cutting-edge approaches such as bacteriophage therapy, antimicrobial peptides, and antibody-antimicrobial conjugates are being explored and advanced through academic research. These novel strategies represent a vital part of the global effort to curb the threat of AMR and ensure effective treatment options for future generations. Thus, the academic sector can provide robust solutions to counter AMR by driving innovative research, such as exploring microbiome dynamics as predictors of treatment success, identifying novel contributors like extracellular vesicles, and advancing cutting-edge technologies like bacteriophage therapy and antimicrobial peptides. These efforts complement the pharmaceutical industry by uncovering foundational knowledge and pioneering alternative approaches that can be scaled for practical applications.
Mansi Jamsudkar
mansi.jamsudkar@mmactiv.com