WHO report: Antibiotic resistance poses serious threat to public health
May 01, 2014 | Thursday | Reports/white papers | By BioSpectrum Bureau
WHO report: Antibiotic resistance poses serious, worldwide threat to public health
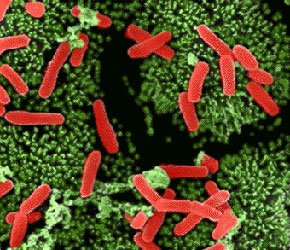
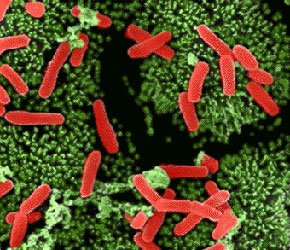
A new report by the World Health Organization (WHO) - the first to look at antibiotic resistance globally mentions that antibiotic resistance that occurs when bacteria change so antibiotics no longer work in people who need them to treat infections, is now a major threat to public health. It reveals that the this resistant bacteria has the potential to affect anyone, of any age, in any country.
"Without urgent, coordinated action by many stakeholders, the world is headed for a post-antibiotic era, in which common infections and minor injuries which have been treatable for decades can once again kill," says Dr Keiji Fukuda, WHO's Assistant Director-General for Health Security. "Effective antibiotics have been one of the pillars allowing us to live longer, live healthier, and benefit from modern medicine. Unless we take significant actions to improve efforts to prevent infections and also change how we produce, prescribe and use antibiotics, the world will lose more and more of these global public health goods and the implications will be devastating."
The report, Antimicrobial resistance: global report on surveillance, notes that resistance is occurring across many different infectious agents but the report focuses on antibiotic resistance in nine different bacteria responsible for common, serious diseases such as bloodstream infections (sepsis), diarrhoea, pneumonia, urinary tract infections and gonorrhoea. The results are cause for high concern, documenting resistance to antibiotics, especially "last resort" antibiotics, in all regions of the world.
Key findings from the report include:
• Resistance to the treatment of last resort for life-threatening infections caused by a common intestinal bacteria, Klebsiella pneumonia - carbapenem antibiotics - has spread to all regions of the world. K. pneumoniae is a major cause of hospital-acquired infections such as pneumonia, bloodstream infections, infections in newborns and intensive-care unit patients. In some countries, because of resistance, carbapenem antibiotics would not work in more than half of people treated for K. pneumoniae infections.
Resistance to one of the most widely used antibiotics for the treatment of urinary tract infections caused by E. coli - fluoroquinolones - is very widespread. In the 1980s, when these drugs were first introduced, resistance was virtually zero. Today, there are countries in many parts of the world where this treatment is now ineffective in more than half of patients.
• Treatment failure to the last resort of treatment for gonorrhea - third generation cephalosporins - has been confirmed in Austria, Australia, Canada, France, Japan, Norway, South Africa, Slovenia, Sweden and the United Kingdom. More than 1 million people are infected with gonorrhoea around the world every day.
• Antibiotic resistance causes people to be sick for longer and increases the risk of death. For example, people with MRSA (methicillin-resistant Staphylococcus aureus) are 64% more likely to die than people with a non-resistant form of the infection. Resistance also increases the cost of health care with lengthier stays in hospital and more intensive care required.